Mark Halsey is a licensed therapist, founder, and chief editor of Clean Break Recovery. With over a decade of addiction treatment experience, Mark deeply understands...Read more
Medicare provides health insurance coverage for millions of Americans, and understanding exactly what it covers can be confusing. One of the most important questions to understand is: What is the Medicare approved amount for mental health services? The answer to this question is vital to ensuring that individuals receive the coverage they need and deserve for mental health services. In this article, we will provide an overview of the Medicare approved amount for mental health services, along with other important information about these services and Medicare coverage.
The Medicare-approved amount is the amount a doctor or provider can be paid for a covered service or item. For mental health services, the Medicare-approved amount may vary depending on the type of service provided and where you receive the care. Generally, Medicare pays 80 percent of the approved amount and you are responsible for the remaining 20 percent. You may also be responsible for any deductibles or coinsurance.
Contents
- What is the Medicare Approved Amount for Mental Health Services?
- What is Medicare?
- What Other Benefits Does Medicare Provide for Mental Health Services?
- Top 6 Frequently Asked Questions
- What is the Medicare Approved Amount for Mental Health Services?
- What is the difference between Medicare Part A and Part B?
- Are there any restrictions on how often I can use Medicare-approved mental health services?
- Does Medicare cover mental health services provided in a hospital setting?
- Do I need a referral from my primary care doctor to get Medicare-approved mental health services?
- Do I need to pay anything out-of-pocket for Medicare-approved mental health services?
What is the Medicare Approved Amount for Mental Health Services?
What is Medicare?
Medicare is a health insurance program administered by the federal government that provides coverage for a variety of medical services and supplies. Medicare is available to individuals who are over the age of 65, certain disabled individuals, and individuals who have end-stage renal disease.
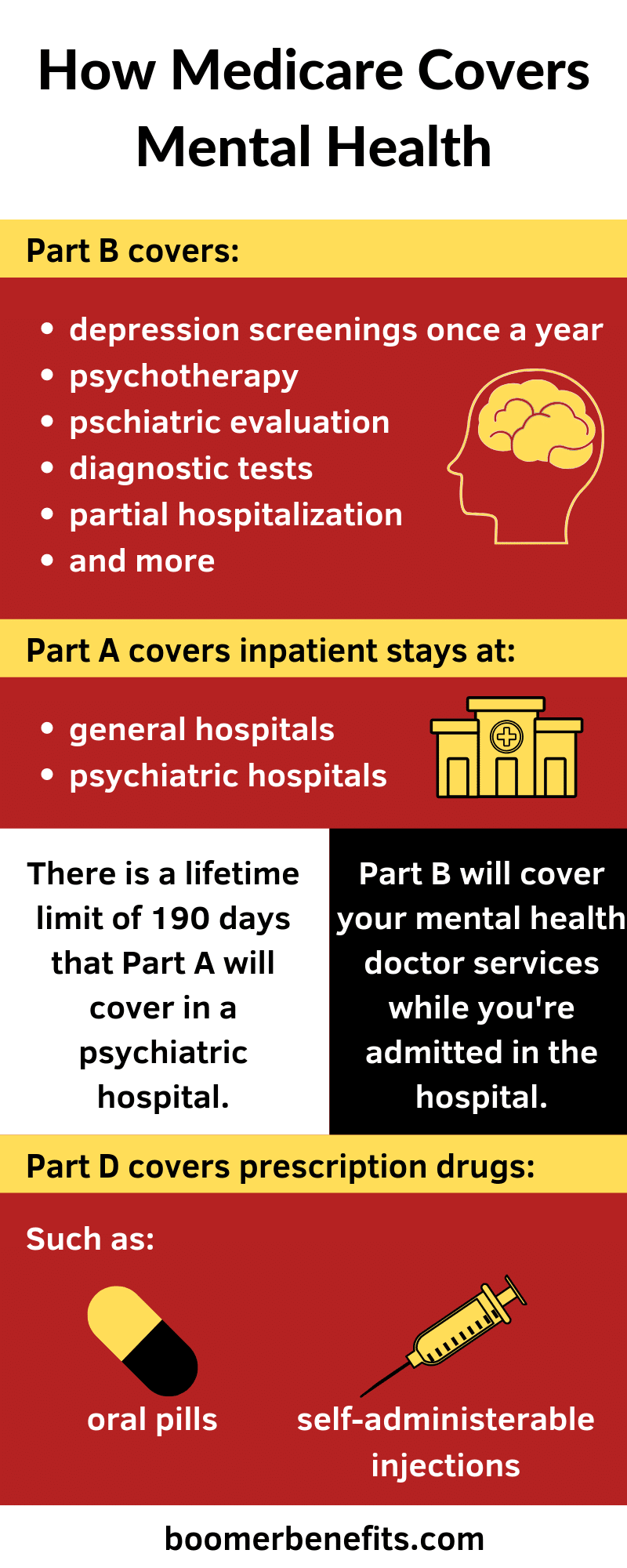
Medicare is divided into four parts: Part A (hospital insurance), Part B (medical insurance), Part C (Medicare Advantage plans), and Part D (prescription drug coverage). Medicare Part B covers a variety of mental health services, including outpatient counseling, psychiatric care, and substance abuse treatment.
What Mental Health Services Does Medicare Cover?
Medicare Part B covers mental health services provided by a qualified healthcare provider. These services include psychotherapy, psychiatric evaluations, and medication management. Medicare also covers laboratory tests related to mental health services, as well as certain medications prescribed for the treatment of mental health conditions.
In addition, Medicare Part B covers certain services related to substance abuse treatment, such as inpatient detoxification, residential treatment, and outpatient counseling. Medicare also covers certain preventive mental health services, such as depression screenings.
How Much Does Medicare Pay for Mental Health Services?
The amount Medicare will pay for mental health services depends on the type of service and the provider that is delivering the service. Most mental health services are subject to Medicare’s deductible and coinsurance requirements. This means that Medicare will pay a portion of the cost of the services, and the patient is responsible for the remaining cost.
For some services, Medicare will pay the full cost of the service. For instance, Medicare covers certain preventive mental health services in full, such as depression screenings and yearly wellness visits. Medicare also covers certain laboratory tests related to mental health services in full.
What Other Benefits Does Medicare Provide for Mental Health Services?
In addition to covering a portion of the cost of mental health services, Medicare also provides additional benefits for those seeking mental health treatment. Medicare Part B covers the cost of mental health services provided in a partial hospitalization program, which is an intensive outpatient treatment program.
Medicare also covers the cost of certain mental health services provided in a residential treatment center. This type of treatment is provided in a facility that is similar to a hospital and is designed to treat individuals with severe mental illnesses.
Does Medicare Cover Mental Health Services Provided by Non-Physician Providers?
Medicare typically only covers mental health services provided by a qualified healthcare provider, such as a psychiatrist, psychologist, or clinical social worker. However, Medicare may cover certain mental health services provided by non-physician providers, such as marriage and family therapists, in certain circumstances.
Medicare also covers certain mental health services provided by non-physician providers in a partial hospitalization program or residential treatment center. The amount Medicare will pay for these services depends on the type of service and the provider that is delivering it.
Does Medicare Cover Mental Health Services Provided in a Group Setting?
Medicare does cover certain mental health services provided in a group setting. These services must be provided by a qualified healthcare provider and must meet Medicare’s criteria for group therapy. The amount Medicare will pay for these services depends on the type of service and the provider that is delivering it.
Top 6 Frequently Asked Questions
What is the Medicare Approved Amount for Mental Health Services?
Answer: Medicare Part B covers 80 percent of the Medicare-approved amount for mental health services such as outpatient visits to a psychiatrist, psychologist, or other mental health care provider. The approved amount is based on the provider’s usual fee and the location where the services are provided. Medicare also covers mental health services provided in a hospital outpatient setting. Medicare Part A covers inpatient mental health services provided in a psychiatric hospital.
What is the difference between Medicare Part A and Part B?
Answer: Medicare Part A covers inpatient hospitalization and other medical services such as skilled nursing care, hospice care, and some home health care. Medicare Part B covers outpatient services such as doctor visits, preventive care, diagnostic tests, and certain medical equipment. It also covers some mental health services such as outpatient visits to a psychiatrist, psychologist, or other mental health care provider.
Are there any restrictions on how often I can use Medicare-approved mental health services?
Answer: Yes, Medicare has limits on how often you can use certain types of mental health services. For example, Medicare Part B covers 80 percent of the approved amount for up to 20 outpatient visits to a psychiatrist or other mental health care provider each year. Your provider may also place limits on the number of visits they can provide each year.
Does Medicare cover mental health services provided in a hospital setting?
Answer: Yes, Medicare Part A covers inpatient mental health services provided in a psychiatric hospital. In addition, Medicare Part B covers mental health services provided in a hospital outpatient setting. Medicare Part B also covers 80 percent of the Medicare-approved amount for outpatient visits to a psychiatrist, psychologist, or other mental health care provider.
Do I need a referral from my primary care doctor to get Medicare-approved mental health services?
Answer: You do not need a referral from your primary care doctor to get Medicare-approved mental health services. However, if you are seeing a mental health care provider for the first time, you may need to get a referral from your primary care doctor or a mental health care provider.
Do I need to pay anything out-of-pocket for Medicare-approved mental health services?
Answer: Yes, you may have to pay something out-of-pocket for Medicare-approved mental health services. Medicare Part B covers 80 percent of the Medicare-approved amount for mental health services. You are responsible for the remaining 20 percent. You may also have to pay a deductible or coinsurance for certain services.
The Medicare Approved Amount for Mental Health Services is a critical part of the care and treatment of those who need and seek mental health services. It provides a safeguard for those who may not be able to afford mental health services, and it helps to ensure that mental health resources are being used appropriately. Knowing and understanding the Medicare approved amount for mental health services can help individuals and health care providers alike in the process of providing quality mental health care.
Mark Halsey is a licensed therapist, founder, and chief editor of Clean Break Recovery. With over a decade of addiction treatment experience, Mark deeply understands the complex needs of those struggling with addiction and utilizes a comprehensive and holistic approach to address them. He is well-versed in traditional and innovative therapies, including cognitive-behavioral therapy, motivational interviewing, and mindfulness-based interventions.
More Posts